The Anthem HealthKeepers website provides a host of self-service tools to help members manage their health benefits. However, if you experience a problem that you cannot handle on your own, you can reach out to Anthem HealthKeepers Plus’ customer support team. They can assist you with issues relating to eligibility, claims status, and provider data updates. They also provide live chat and can help you resolve payment disputes. For more complex issues, you can contact the Provider Experience team, which will respond to your questions or concerns within two business days.
Sponsorships of anthem health keepers
Anthem Blue Cross and Blue Shield is an insurance company that helps people live healthier life. In 2014, they directed $3.3 million toward health-improving causes, and hundreds of employees volunteered their time to support these causes. They focus their efforts on promoting healthy lifestyles and reducing the debilitating impact of chronic illnesses and diseases.
The company’s corporate team has long supported the American Lung Association, including sponsoring the Wisconsin Fight for Air Climb. Since 2009, the corporate team has raised tens of thousands of dollars for the cause. This year, they expect to raise $725,000 for the cause through corporate sponsorship and individual fundraising.
Learn more about: How to boost your immune system naturally as winter approaches?
Plan features
The Anthem Healthkeepers plan offers a number of benefits, including a mobile app. This app will help you find a doctor, check your benefits, and ask questions. In addition, you can access digital ID cards and check your plan benefits on the go. However, some members of the Anthem health insurance network have complained about the denial of claims and poor customer service.
Plan doctors
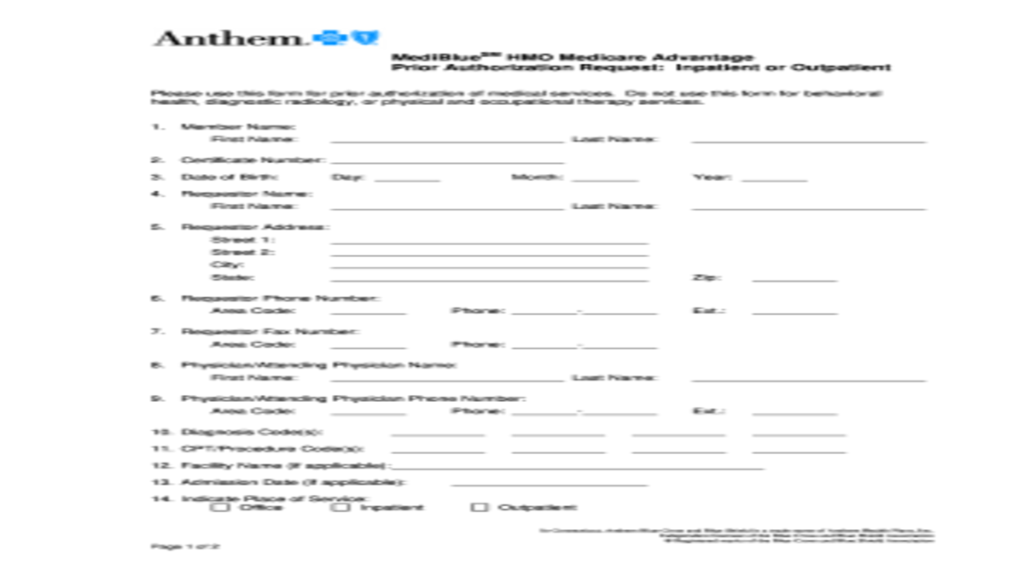
Anthem has a network of healthcare providers and facilities. These include physicians, specialists, hospitals, pharmacies, urgent care centers, and labs. They are known as in-network or preferred providers and work with the insurer to ensure the best care possible for their clients. These providers can also assist with claims and preapprovals.
Plan self-service tools
Anthem Blue Cross offers several self-service tools for health plan members. Whether you need to pay your bill or update provider data, the self-service tools offered by Anthem can handle most of your issues. When you have a more complex problem or need assistance, you can always contact an associate through live chat or a secure site. You can also contact the Provider Experience team, which will respond to your inquiries within two business days.